Cannabis has emerged as a strong favorite for new potential therapeutic agents in the treatment of autoimmune disorders due to its interaction with the endocannabinoid system, which plays a role in regulating immune responses.
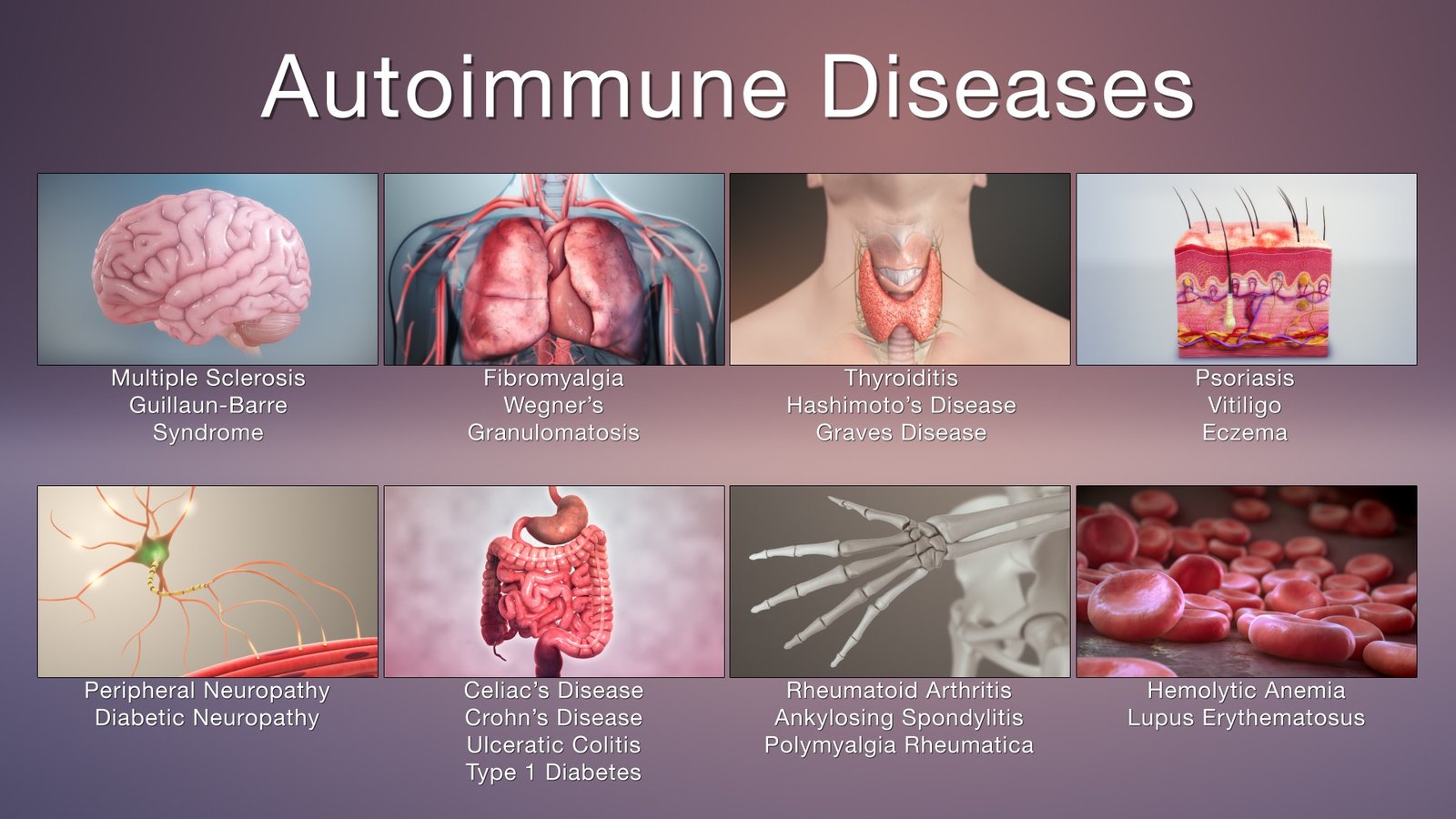
Autoimmune conditions, such as multiple sclerosis, rheumatoid arthritis, and inflammatory bowel disease, occur when the immune system mistakenly attacks the body’s own tissues, leading to chronic inflammation, tissue, and nerve damage. Cannabinoids like THC and CBD exhibit anti-inflammatory and immunomodulatory properties that may help reduce overactive immune responses. Research has shown that cannabinoids can suppress the production of pro-inflammatory cytokines and promote regulatory mechanisms that may alleviate symptoms like pain, swelling, and fatigue commonly experienced by patients with autoimmune diseases.
To speak in plainer language. I have used nothing but cannabis products to treat my Multiple Sclerosis. It’s been nearly five years now, and I shock many Doctors! They see my MRIs and the length of time since diagnosis and call me fortunate!
I was originally diagnosed by the Cleveland Clinic and started treatment right away. I took 1 pill twice a day, and the cost was $12,500 per month. The side effects were in some ways as bad as the MS. Over time, my labs deteriorated, and it appeared the medication was killing me. Instead of stopping all medication for several months and then trying the next greatest thing, I decided to try cannabis.
I first used marijuana at the age of 15. I used marijuana regularly for several years and then off and on in my 30s. I knew about recreational marijuana, but I knew nothing about the different cannabinoids and strains, and cannabis as medicine. I learned fast. I am a researcher type and studied and read and learned and experimented all I could. The result, five years later, I believe I have cracked the code! I know what works for me and many others. I know what doesn’t work and I know why. I have learned what each cannabinoid does and how to effectively use it in treatments. I have found ratios of cannabinoids that are more effective together than isolated. Over 50 people in our county who have an autoimmune disorder or chronic pain are using my products to find relief for their symptoms. I am not interested in recreational users as customers. I am interested in people who suffer chronically because I know my products can help.
THE DEEP DIVE
Autoimmune diseases affect millions of people worldwide, creating chronic inflammation, pain, and immune system dysfunction that can significantly reduce quality of life. Traditional treatments, such as corticosteroids and immunosuppressive drugs, often come with serious side effects, including increased infection risk, liver damage, and dependency. In recent years, medical cannabis has emerged as a promising complementary therapy for autoimmune patients due to its anti-inflammatory, analgesic, and immunomodulatory properties. By influencing the body’s endocannabinoid system, cannabis offers a natural, multifaceted approach to managing autoimmune symptoms while supporting overall well-being.
The human body contains an intricate network known as the endocannabinoid system, which regulates immune response, mood, pain, and inflammation. The ECS consists of receptors—primarily CB1 and CB2—that interact with cannabinoids, both those produced naturally by the body and those introduced through cannabis. THC and CBD are the two most well-known cannabinoids, each playing distinct yet complementary roles in therapeutic use. THC binds primarily to CB1 receptors in the brain and nervous system, reducing pain perception and stimulating appetite, while CBD interacts with CB2 receptors in immune cells, helping modulate inflammation and prevent overactive immune responses. For autoimmune patients—whose immune systems mistakenly attack healthy tissues—this regulation can be life-changing.
Research has demonstrated that cannabinoids possess powerful anti-inflammatory and immunosuppressive effects. For instance, in conditions like rheumatoid arthritis, lupus, multiple sclerosis, and Crohn’s disease, cannabis can help reduce cytokine production—molecules responsible for triggering inflammation. A 2019 study published in Frontiers in Immunology found that cannabinoids suppress the activation of inflammatory pathways and decrease oxidative stress, leading to reduced tissue damage in autoimmune disorders. By dampening this overactive immune response, cannabis helps restore balance without completely shutting down immune function, unlike many pharmaceutical immunosuppressants.
Pain relief is another major benefit for autoimmune patients using cannabis. Chronic pain from inflammation, nerve damage, or muscle stiffness can severely limit daily activities and emotional health. Cannabinoids, particularly THC, work synergistically with the body’s natural pain control systems to reduce both neuropathic and inflammatory pain. A 2021 clinical review in Pain Medicine concluded that medical cannabis can be an effective adjunct or alternative to opioid therapy, providing comparable pain relief with significantly fewer risks of addiction and overdose. For patients with fibromyalgia or multiple sclerosis, cannabis has also been shown to improve muscle relaxation, reduce spasms, and enhance sleep quality—factors that contribute directly to better quality of life.
Beyond physical relief, cannabis also offers important psychological and emotional benefits for autoimmune patients. Chronic illnesses often lead to depression, anxiety, and insomnia, partly due to constant pain and uncertainty. CBD, in particular, has been widely studied for its anxiolytic (anxiety-reducing) and antidepressant properties. By interacting with serotonin receptors and promoting neurogenesis, CBD helps stabilize mood and reduce anxiety without the side effects commonly associated with psychiatric medications. Moreover, many patients report improved sleep patterns when using cannabis, which is essential for immune regulation and tissue repair. Adequate rest allows the body to better manage autoimmune flare-ups and maintain a more balanced immune system.
An equally important advantage of medical cannabis is its versatility and personalization. Patients can choose from various delivery methods—including tinctures, capsules, edibles, and topical creams—depending on their symptoms and tolerance. Those with gastrointestinal autoimmune conditions, such as Crohn’s or ulcerative colitis, often prefer oral tinctures or capsules for systemic relief, while topical applications can target localized inflammation in conditions like psoriasis or arthritis. Furthermore, different cannabis strains and cannabinoid ratios allow for precise symptom management. For example, high-CBD, low-THC strains may be ideal for daytime use, offering relief without psychoactive effects, whereas balanced strains may provide deeper pain and sleep support.
Despite lingering stigma and inconsistent legal status, the growing body of scientific evidence supports the inclusion of medical cannabis as a legitimate therapeutic option for autoimmune patients. States that have legalized medical cannabis programs have reported reductions in opioid prescriptions, hospital admissions, and reliance on traditional pharmaceuticals. This shift not only benefits individual patients but also alleviates strain on healthcare systems. Continued research and policy reform are necessary to expand access, improve product quality standards, and integrate cannabis-based therapies into mainstream medical practice.
In conclusion, cannabis represents a powerful, natural alternative for patients struggling with autoimmune diseases. Through its regulation of the endocannabinoid system, it reduces inflammation, alleviates pain, and promotes emotional stability—without the harsh side effects associated with many conventional medications. As scientific understanding deepens, cannabis is increasingly being recognized not as a last resort, but as a cornerstone of holistic autoimmune care. For millions of patients seeking relief and restored quality of life, medical cannabis offers not only symptom management but also hope for a more balanced and sustainable approach to healing.